With the reality of value-based purchasing settling in, over the past several months I’ve had the same conversation with a number of healthcare executives related to H-CAHPS performance. In describing their efforts, they explain, “We’ve set specific goals; we’ve clearly identified standards on checklists for each H-CAHPS dimension; and we’re rounding with purpose more often to monitor compliance, but ….”
“But your scores aren’t changing?” I interrupt.
“Exactly. How did you know?”
Each healthcare organization’s journey to improve the patient experience and resultant H-CAHPS scores is unique, with many factors influencing performance. But a common problem I hear from many frustrated executives revolves around the mistaken hope that applying tried-and-true approaches that are designed to change discreet, tactical procedures – the kind that lend themselves to checklists – also will change aspects of the culture that support improved H-CAHPS results.
Exacerbating the problem is the natural response to disappointing performance when you use checklists. Assuming that better hardwiring and stricter compliance is the answer, managers pressure staff to adhere to the checklist, which usually heightens frustration and discouragement. The downward spiral of employee dissatisfaction makes progress on the patient experience measures in H-CAHPS nearly impossible.
The recent experience of one hospital provides of stark example of how an organization can perform exceptionally well on process measures but struggle mightily on improving the overall patient experience.
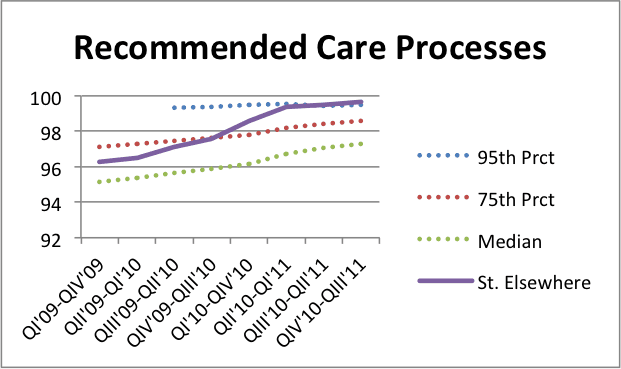
Data in the following two graphs is taken from “Why Not the Best?” (www.whynotthebest.org), the not-for-profit Commonwealth Fund’s healthcare improvement portal, which is arguably the most robust, user-friendly place on the web to access and understand CMS provider scores. Graph 1 trends the composite care process scores of “St. Elsewhere,” an anonymous but real hospital’s current results. The institution’s progress in improving care process compliance is remarkable, moving from below the 75th percentile just a couple of years ago to above the benchmark 95th percentile in the most recent reporting period.
One might expect an institution’s ability to move performance this rapidly on care process measures would translate to superior performance across the board. But the second graph tells a different story. For the past several years, this hospital has struggled well below the threshold 50th percentile rank on H-CAHPS scores. (Remember that institutions scoring below the median of all hospitals receive no points in value-based purchasing scoring methodology.)
 While there are surely many factors contributing to this hospital’s results, the data do demonstrate that achieving success in process does not translate directly to success in patient experience as measured by H-CAHPS.
While there are surely many factors contributing to this hospital’s results, the data do demonstrate that achieving success in process does not translate directly to success in patient experience as measured by H-CAHPS.
So what’s really at the heart of this dichotomy? To understand the problem with using a checklist mentality to improve patient experience scores, let’s look at a few of the specific questions from both the Care Process Measures and H-CAHPS sections from value-based purchasing.
- For AMI patients, fibronolytic therapy received within 30 minutes of arrival? “Check.”
- For pneumonia patients, blood cultures performed in the ED prior to initial antibiotic? “Check.”
- For surgical patients, prophylactic antibiotic received within one hour of incision? “Check.”
Process measures are well defined and straightforward. But when you try to apply that same checklist methodology to H-CAHPS questions, compliance plays out in a very different way that doesn’t lend itself to a simple “check, complete, move-on” mentality.
- Did we (specifically, nurses and doctors) always explain things in a way that patients could understand? “I gave them the required information. I think they understood.”
- Did we always listen carefully to patients? “I tried to listen … most of the time … I think.”
- Did we always do everything we could to help with pain? “I told her to push her call light when she needed more pain medication.”
These examples highlight three major differences between H-CAHPS and care process scores that organizations must understand and address to make real, sustainable progress in patient experience improvement.
How, not just what
While process improvement is about doing the right things, patient experience improvement is more about doing things right. How hospitals implement clinical staff hourly rounding programs, for example, provides a great case study. Staff can enter the patient’s room, assess the required four Ps (pain, position, “potty,” and possessions) on the checklist, and then document compliance. But if they haven’t communicated effectively and connected with the patient on a personal level, the positive impact of hourly rounding is questionable.
Every patient, every hour, every encounter
Remember that the performance standard for most H-CAHPS questions is expressed in how often the practice or behavior was experienced by patients, with “Always” being the top-box response that counts in value-based purchasing scoring. Checklists work for discrete, single-incident compliance; consistent behaviors like those measured in H-CAHPS demand changes in organizational culture and peer-to-peer accountability.
Talents, not just tactics
At the heart of a majority of H-CAHPS measures is effective interpersonal communication. Assuming that all staff naturally possess the skills to communicate effectively is naïve, especially when we know that many communication encounters with patients and their families are under stressful, difficult circumstances. Just as we educate staff to ensure clinical competence, investing in staff development to build superior communication competencies supports higher performance in patient experience, patient safety and employee engagement.
Checklists are effective in standardizing performance and ensuring compliance in many care processes. But expecting them to change organizational culture and the overall patient experience is akin to prescribing a great medication when what the patient really needs is surgery.
Smart leadership teams understand the need to build a robust toolbox of diverse approaches to improve all aspects of organizational performance. Equipping staff with both the tactics and the competencies to achieve success is essential in healthcare’s move from volume to value.

