Effective January 1, 2016, Medicare now pays physicians and non-physician practitioners for time spent providing face-to-face advance care planning (ACP).
 *From the CPT Coding Manual
*From the CPT Coding Manual
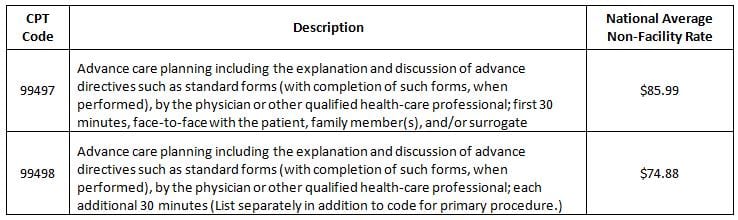
For the sake of comparison, payment for ACP is about 20% less than payment for a level-4 established patient office visit (CPT code 99214), which requires 25 minutes of face-to-face time with the patient, if coded based on time.
In the 2016 Medicare Physician Fee Schedule Final Rule, CMS gave the following directions on providing and billing for ACP, while also promising to publish additional sub-regulatory guidance in the near future:
WHO?
- Primary care physicians and specialists may bill for ACP. Unlike transitional care management (TCM) (CPT codes 99495 and 99496) or chronic care management (CCM) (CPT code 99490), more than one provider may bill for ACP furnished to the same patient during the same time period.
- ACP may be billed by physicians and non-physician practitioners (NPP) only. However, ACP may be furnished incident to the services of the billing physician or NPP, meaning other clinical staff may perform the service under the direct supervision of the physician or NPP. All requirements for “incident to” billing must be met, and the clinical staff providing the service must be qualified under state licensure laws.
- ACP is a stand-alone billable visit in a rural health clinic (RHC) or Federally Qualified Health Center (FQHC), when furnished by an RHC or FQHC practitioner and if all other program requirements are met. However, if ACP is furnished on the same day as another billable visit at an RHC or FQHC, only one visit will be paid.
WHAT?
- Completion of relevant legal forms is not a required element of ACP. However, time spent reviewing and discussing advance directives is included in the service. The CPT manual defines an advance directive as “a document appointing an agent and/or recording the wishes of a patient pertaining to his/her medical treatment at a future time should he/she lack decisional capacity at that time.” This includes, for example, a healthcare proxy, durable power of attorney for healthcare, living will, and medical orders for life-sustaining treatment.
- While CMS will evaluate whether a national coverage determination should be developed for ACP, for the time being, the Medicare Administrative Contractors (known as MACs) will be responsible for local coverage decisions.
WHEN?
- CPT code 99497 may be billed for the first 30 minutes of services on a given day, and CPT code 99498 may be billed for each additional30 minutes of service performed on the same day, with no limit. For example, for a meeting lasting an hour-and-a-half, a physician would bill one unit of 99497 and two units of 99498. There are no frequency limitations to these codes, so they may be used as often as the need arises.
- The ACP codes also may be billed on the same day as most other inpatient and outpatient evaluation and management (E/M) codes, provided that the time counted to bill the ACP codes is only counted for ACP services, and not also used to meet time-based criteria for an E/M code.
- A physician or NPP may bill for ACP furnished during the same time period the physician or NPP is providing TCM or CCM.
- ACP may be furnished in conjunction with a Welcome to Medicare visit or an annual wellness visit. In these instances, Medicare provides first-dollar coverage for the service (when billed with modifier -33). In all other instances, ACP is subject to cost-sharing requirements.
WHERE?
- ACP may be furnished in a variety of settings, including inpatient, an outpatient clinic, and the patient’s home. In the 2016 Hospital Outpatient Prospective Payment System Final Rule, CMS has established the rules for a hospital to bill for ACP when furnished in a hospital outpatient department.
- Presently, ACP is not reimbursable if furnished via telehealth.
HOW?
- There are no specific performance standards, special training, or quality measures a physician or NPP must satisfy to bill for ACP.
- Unlike chronic care management, the physician or NPP is not required to obtain the patient’s written consent to bill for ACP. Although not required, CMS encourages providers to inform patients of applicable cost-sharing requirements.
- Because ACP is a time-based code, the documentation must include the total amount of time spent face-to-face with the patient, family members, and/or surrogate. For auditing purposes, start and stop times are the preferred – but not required – method of documentation.
PYA can assist your organization in developing and implementing a successful and compliant ACP program. For more information, contact Lori Foley (lfoley@pyapc.com) or Martie Ross (mross@pyapc.com) at (888) 420-9876.


